Proximal Hamstring Tendinopathy Exercises: A Comprehensive Guide
This guide details rehabilitation and prevention strategies for proximal hamstring tendinopathy (PHT), offering a PDF resource for optimized exercise prescription and tendon remodeling, crucial for athletes and active individuals.
Understanding Proximal Hamstring Tendinopathy (PHT)
Proximal Hamstring Tendinopathy (PHT) represents a challenging condition affecting the hamstring tendons where they attach to the ischial tuberosity – the ‘sit bone’. Unlike acute hamstring strains, PHT is a degenerative process, often developing gradually over time due to repetitive strain and overload. It’s crucial to differentiate this from a muscle strain, as treatment approaches differ significantly.

This condition commonly impacts runners and endurance athletes, though footballers are also susceptible. The hamstrings, comprised of three muscles sharing a common origin, are vital for propulsion. PHT isn’t simply inflammation; it involves structural changes within the tendon itself. Understanding this distinction is key to effective rehabilitation, often detailed in resources like a PDF guide focusing on proximal hamstring tendinopathy exercises. Ignoring early symptoms can lead to chronic pain and functional limitations, hindering athletic performance and daily activities.
Causes and Risk Factors of PHT
Several factors contribute to the development of Proximal Hamstring Tendinopathy (PHT). Repetitive strain, particularly during activities involving forceful hip extension and knee flexion – like running and sprinting – is a primary cause. Insufficient warm-up routines and inadequate flexibility can also predispose individuals to this condition. Muscle imbalances, specifically weakness in the glutes and core, place increased stress on the hamstring tendons.
Training errors, such as rapid increases in intensity or volume, are significant risk factors. Anatomical variations and biomechanical inefficiencies can also play a role. A comprehensive PDF resource on proximal hamstring tendinopathy exercises will often emphasize addressing these underlying issues. Understanding these causes is vital for preventative strategies and targeted rehabilitation programs, minimizing the risk of chronic pain and ensuring a safe return to activity.
Symptoms of Proximal Hamstring Tendinopathy
Proximal Hamstring Tendinopathy (PHT) typically presents as deep, aching pain in the buttock region, often localized to the ischial tuberosity – the “sit bone.” Pain is frequently aggravated by activities like running, sprinting, prolonged sitting, and even climbing stairs. Initially, symptoms may be mild and activity-related, but can progress to constant, debilitating pain if left unaddressed.
Tenderness to palpation over the hamstring origin is a common finding. Stiffness in the hamstring muscles is also frequently reported. A detailed PDF guide on proximal hamstring tendinopathy exercises will highlight differentiating PHT from other conditions like sciatica or hamstring strains. Recognizing these symptoms early is crucial for initiating appropriate rehabilitation and preventing the condition from becoming chronic, allowing for a focused exercise approach.

Diagnosis of PHT
Accurate diagnosis, often utilizing MRI or ultrasound (detailed in a PDF), is essential to differentiate PHT from other conditions and guide targeted exercise interventions.
Physical Examination Techniques
A thorough physical examination is the cornerstone of PHT diagnosis, often preceding imaging. Palpation around the ischial tuberosity helps identify tenderness, a key indicator. Specific tests, like the hamstring loading test, assess pain provocation during contraction. PDF resources detail these techniques.
Range of motion assessments evaluate hamstring flexibility and identify limitations. Neurological screening rules out nerve involvement. Strength testing compares affected and unaffected sides, revealing deficits. Functional assessments, observing movements like walking or running, highlight compensatory patterns. Understanding muscular forces, as outlined in downloadable PDFs, informs test interpretation.

Clinicians must correlate examination findings with patient history to establish a diagnosis. Precise assessment guides exercise selection, optimizing rehabilitation protocols. A comprehensive examination, supplemented by PDF guides, ensures accurate identification and targeted treatment of PHT.
Imaging Modalities (MRI, Ultrasound)
While clinical examination is primary, imaging confirms PHT diagnosis and assesses severity. Magnetic Resonance Imaging (MRI) provides detailed views of the hamstring tendons, revealing structural changes like tendinosis or tears. PDF resources often include MRI interpretations. Ultrasound, a more accessible option, dynamically assesses tendon thickness and integrity during movement.
MRI excels at identifying fluid within the tendon, indicating inflammation or degeneration. Ultrasound is useful for guiding injections and monitoring treatment progress. Both modalities help differentiate PHT from other conditions, like hamstring strains. Downloadable PDFs illustrate typical imaging findings.
Imaging guides rehabilitation planning, informing load management and exercise progression. It’s crucial to correlate imaging results with clinical findings for accurate diagnosis and treatment. Accessing PDF guides enhances understanding of imaging interpretations and their implications for exercise prescription.

Exercise-Based Rehabilitation for PHT
A structured exercise program is central to PHT recovery, progressing through phases focusing on pain management, strengthening, and functional movements – PDF guides detail each stage.
Phase 1: Pain Management & Isometric Exercises
Initial rehabilitation focuses on controlling pain and initiating gentle muscle activation. Isometric exercises are foundational, involving hamstring contractions without joint movement, minimizing stress on the injured tendon. A PDF resource will demonstrate proper form for isometric hamstring contractions, holding for 5-10 seconds, repeated several times throughout the day.
Alongside this, pelvic tilts and core stabilization exercises are crucial. These enhance neuromuscular control and support the pelvis, indirectly reducing load on the hamstring tendon. These exercises, also detailed in the PDF, promote a stable base for subsequent strengthening. The goal is to establish a pain-free foundation before progressing to more dynamic movements, ensuring optimal tendon healing and preventing re-injury.
Remember, pain is a guide; any increase in symptoms necessitates modifying the exercise or reducing intensity.
Isometric Hamstring Contractions
Isometric hamstring contractions are a cornerstone of Phase 1 rehabilitation, detailed within the accompanying PDF guide. These exercises involve activating the hamstring muscles without changing their length, minimizing stress on the proximal tendon. Begin in a comfortable position – lying prone, seated, or standing with slight knee bend.
Focus on consciously squeezing the hamstring muscles as if attempting to bend the knee, but resist the movement. Hold this contraction for 5-10 seconds, then relax. Repeat 8-12 times, several sets throughout the day. The PDF provides visual demonstrations and modifications for varying pain levels.
Crucially, maintain proper form and avoid holding your breath. Monitor pain levels; contractions should be pain-free or cause minimal discomfort. This exercise builds foundational strength and prepares the tendon for more demanding loads.
Pelvic Tilts & Core Stabilization
Alongside isometric hamstring work, pelvic tilts and core stabilization are vital in Phase 1, as outlined in the comprehensive PDF resource. A strong core provides a stable base for hamstring function, reducing compensatory strain on the proximal tendon. Begin lying supine with knees bent and feet flat on the floor.
Gently tilt your pelvis backward, flattening your lower back against the floor, then tilt forward, creating a small arch. Focus on controlled movements, engaging your abdominal muscles throughout. Perform 10-15 repetitions. The PDF details progressions, including adding resistance with a stability ball.
Core stabilization exercises, like drawing-in maneuvers, further enhance stability. These exercises improve neuromuscular control and protect the injured tendon during functional activities. Remember to breathe deeply and maintain proper form.
Phase 2: Strengthening Exercises
Transitioning from pain management, Phase 2 focuses on restoring hamstring strength, as detailed in the PDF guide. This phase introduces progressive loading to stimulate tendon adaptation and improve functional capacity. Begin with exercises that minimize stress on the proximal tendon, gradually increasing intensity.
Key exercises include Nordic hamstring curls, glute bridges, and modified Romanian deadlifts (RDLs). The PDF provides detailed instructions on proper technique and progression for each exercise. Nordic curls, performed with a partner, eccentrically load the hamstrings, promoting tendon remodeling.
Glute bridges and RDLs strengthen the posterior chain, supporting hamstring function. Modifications, such as reduced range of motion in RDLs, are crucial to avoid exacerbating symptoms. Consistent adherence to the program, guided by the PDF, is essential for optimal results.
Nordic Hamstring Curls (Progression & Technique)
The Nordic hamstring curl is a highly effective, yet challenging, exercise detailed within the PDF guide for PHT rehabilitation; It focuses on eccentric hamstring strength, crucial for tendon rehabilitation. Proper technique is paramount to prevent injury; a partner is required for stabilization.
Begin with a supported Nordic curl, using a foam pad under the ankles and a partner holding the upper thighs. Slowly lower the body towards the ground, controlling the descent with the hamstrings. The PDF outlines a progression – starting with a minimal range of motion and gradually increasing it as strength improves.

Focus on a slow, controlled eccentric phase, avoiding rapid movements. If unable to return to the starting position, the partner assists. The PDF emphasizes starting with 3-5 repetitions and gradually increasing sets and reps. This exercise, when performed correctly, significantly enhances hamstring strength and resilience.
Glute Bridges & Hip Extensions
Glute bridges and hip extensions are foundational exercises, thoroughly explained in the PDF guide, for addressing PHT. These movements strengthen the gluteal muscles and hamstrings, promoting hip extension and reducing stress on the proximal hamstring tendon. They are excellent starting points for rehabilitation.
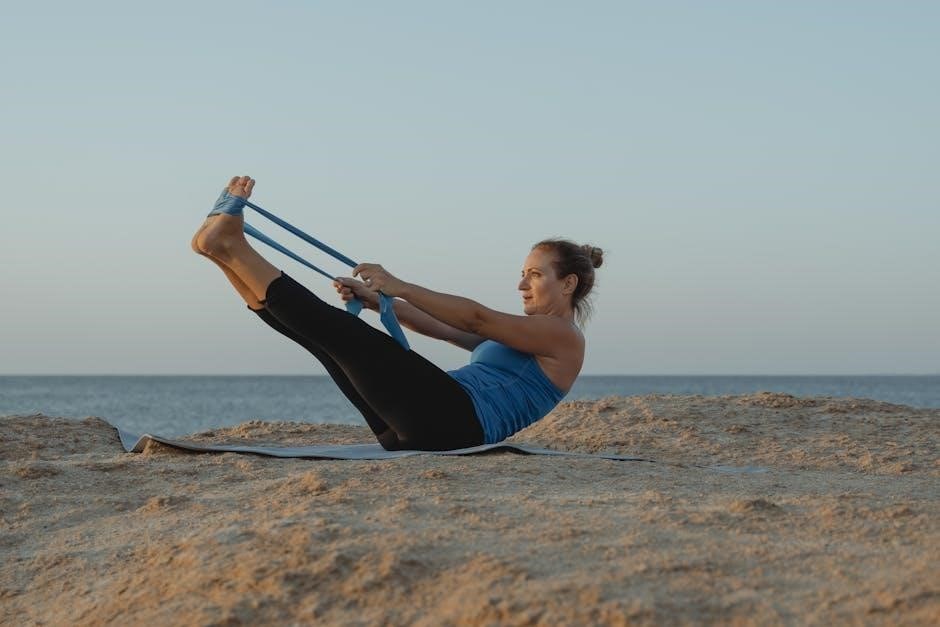
Begin with glute bridges, lying supine with knees bent and feet flat on the floor. Lift the hips off the ground, squeezing the glutes at the top. The PDF details progressions, including single-leg glute bridges for increased challenge. Hip extensions can be performed using a machine or with resistance bands.
Focus on controlled movements and maintaining proper form. The PDF stresses avoiding lower back arching. Incorporate 3 sets of 10-15 repetitions, gradually increasing resistance as strength improves. These exercises build a solid base for more advanced PHT rehabilitation protocols.
Romanian Deadlifts (RDLs) ─ Modified for PHT
Romanian Deadlifts (RDLs), as detailed in the PDF, are crucial for hamstring and gluteal strengthening, but require careful modification for PHT. Traditional RDLs can exacerbate pain; therefore, a reduced range of motion is essential. Focus on a slight bend in the knees throughout the movement, maintaining a neutral spine.
The PDF emphasizes initiating the movement from the hips, pushing them backward while keeping the back straight. Lower the weight (dumbbells or barbell) only to a comfortable point before feeling hamstring tension. Avoid rounding the back or excessive stretching.
Start with lighter weights and higher repetitions (3 sets of 12-15). The PDF provides guidance on progressively increasing the load as pain subsides and strength improves. Proper form is paramount to prevent re-injury and promote effective tendon rehabilitation.
Phase 3: Functional Exercises & Return to Activity
Phase 3, outlined in the PDF, bridges rehabilitation and sport-specific demands. This stage focuses on integrating strength gains into functional movements, preparing for a return to activity. Single-leg Romanian Deadlifts enhance stability and hamstring control, progressing from bilateral RDLs.
Lunges and split squats are introduced cautiously, starting with shallow depths and controlled movements. The PDF details progression criteria, emphasizing pain-free execution. Low-impact plyometrics, like box step-ups, improve power and reactivity without excessive stress on the tendon.
Gradual return to sport is paramount, following a structured plan detailed in the PDF. This includes increasing training volume and intensity incrementally, monitoring for any symptom flare-ups. Prioritizing proper warm-up and cool-down routines is vital for sustained recovery.
Single-Leg Romanian Deadlifts
Single-leg Romanian Deadlifts (SLRDLs), detailed in the PDF, are a cornerstone of Phase 3, enhancing hamstring strength and stability. Begin with bodyweight, focusing on maintaining a neutral spine and controlled hip hinge. The PDF emphasizes a slight bend in the supporting knee to avoid hyperextension.
As strength improves, add light dumbbells or kettlebells, progressing gradually. Monitor for any pain at the hamstring origin; modifications are outlined in the PDF. Maintaining core engagement throughout the movement is crucial for stability. The PDF illustrates proper form and common errors to avoid.
Focus on eccentric control during the lowering phase, resisting gravity. This strengthens the hamstring tendon and prepares it for functional demands. The PDF provides specific rep and set recommendations based on individual progress.
Lunges & Split Squats (Progression)
Lunges and split squats, detailed within the PDF resource, build lower body strength and functional stability, crucial for returning to activity; Start with static lunges, ensuring proper alignment and controlled movement. The PDF highlights maintaining a 90-degree angle in both knees during the exercise.
Progress to dynamic lunges, focusing on smooth transitions and core engagement. Split squats offer a similar challenge with increased stability demands. The PDF outlines regressions for those with limited range of motion or pain. Adding weight—dumbbells or a barbell—should be gradual, as detailed in the PDF.
Pay close attention to hamstring sensation; modify or regress if pain arises. The PDF emphasizes proper warm-up and cool-down routines to optimize recovery and minimize risk of flare-ups.
Plyometric Exercises (Low-Impact)
Low-impact plyometrics, as detailed in the PDF guide, are introduced in the later stages of rehabilitation to enhance power and reactivity. Begin with exercises like box step-ups and lateral step-overs, focusing on controlled landings and minimal joint stress. The PDF stresses the importance of proper technique to avoid exacerbating the tendinopathy.
Progress gradually to exercises like shallow box jumps and split squat jumps, ensuring adequate hamstring strength and pain-free movement. The PDF provides specific guidelines on jump height and repetition schemes. Monitoring pain levels is crucial; any increase warrants regression.
The PDF emphasizes that these exercises should be incorporated only after achieving sufficient strength and control in previous phases. Prioritize quality over quantity, and always include a thorough warm-up and cool-down.

Important Considerations & Precautions

The PDF highlights careful load management and pain monitoring as vital, alongside progression criteria, to prevent flare-ups during rehabilitation for PHT.
Load Management & Pain Monitoring
Effective rehabilitation, detailed in the PDF, necessitates meticulous load management. Initially, exercises should be performed within a pain-free range, gradually increasing intensity and volume. Monitoring pain levels – both during and after exercise – is paramount. A general guideline is to avoid exacerbating symptoms beyond a mild, tolerable discomfort (typically 2-3/10 on a pain scale).
Sudden increases in load or activity can provoke flare-ups, hindering progress. The PDF emphasizes a progressive overload approach, where increases are small and incremental. Pay attention to the body’s response; if pain increases significantly, reduce the load or modify the exercise. Consistent self-assessment and adjustments are key to successful tendon remodeling and preventing re-injury. Remember, respecting pain signals is crucial for long-term recovery.
Progression Criteria & Avoiding Flare-Ups
The accompanying PDF outlines specific progression criteria for each exercise phase. Advancement should only occur when you can perform the current exercise with good form and minimal pain (under 3/10). Key indicators include improved strength, increased range of motion, and reduced pain during functional activities.
Avoiding flare-ups requires adherence to these guidelines and recognizing warning signs. These include a significant increase in pain, swelling, or stiffness. If a flare-up occurs, immediately reduce the load, regress to a previous exercise phase, and address any contributing factors. The PDF stresses the importance of patience and consistency; rushing progression can jeopardize recovery. Prioritize proper technique over lifting heavier weights or performing more repetitions.

Resources & Further Information (PDF Downloads)
Downloadable PDF resources are provided to supplement this guide, offering detailed exercise protocols and a comprehensive rehabilitation program for proximal hamstring tendinopathy (PHT). These PDFs include printable exercise sheets with illustrations, progression guidelines, and pain monitoring scales. The rehabilitation PDF focuses on optimizing muscle strength and function deficits, commonly prescribed for individuals experiencing PHT.
Further information regarding muscular forces and adaptations with hamstring-specific exercises can be found within the downloadable PDF. The prevention PDF details strategies to minimize the risk of recurrence. Access these valuable resources to enhance your understanding and optimize your recovery journey. These PDFs are designed to empower you with the knowledge and tools needed for successful PHT management.